The Ultimate Guide to COPD
Introduction
Shortness of breath, tightness of chest, wheezing, and more. Chronic obstructive pulmonary disease (COPD) is defined by the CDC as “a group of diseases that cause airflow blockage and breathing-related problems” (CDC,2023). Analogous to how dementia covers a wide array of memory conditions, COPD does the same for breathing difficulty conditions. COPD makes breathing difficult for and affects over 16 million Americans with a variety of diagnoses but shared symptoms. However, for a condition that affects so many, there are still burning questions for the average person about how it affects the body and the person’s mind. In this article, we aim to tell you more about both so you can better assist yourself, or your loved one living with the condition.
Emphysema
Emphysema is a COPD condition that develops over and involves the gradual damage of lung tissue. Specifically, Emphysema relates to the “destruction of the alveoli” which are the air sacs in your lungs (ALA, 2023). This condition is often called the most preventable respiratory disease because of its link to smoking. This includes tobacco smoke and marijuana smoke, along with continued secondhand exposure. While some air pollutants (continued occupational exposure to fumes or dust) and other respiratory infections can lead to emphysema its number one cause remains to be smoking. Since this is a gradual disease it can take years to develop symptoms, the degree of onset also varies depending on the level of smoking. Early signs are shortness of breath, coughing with mucus, wheezing, and tightness of the chest. There are several tests that are needed to diagnose if a COPD condition is emphysema specifically. These include “x-rays, pulse oximetry, spirometry and other pulmonary function tests, arterial blood gas tests and electrocardiograms (ECG)” (ALA, 2023). Emphysema can also lead to the development of other conditions. These induce collapsed lungs (pneumothorax), heart problems, and the development of large hotels in the lungs called bullae. Sadly emphysema, like other COPD conditions, cannot be cured but treatments are available to alleviate symptoms. Such as medications, therapies, and surgeries.
Chronic Bronchitis
Chronic bronchitis is “long-term inflammation of the bronchi” which are the breathing tubes in your lungs and airways (JHM, 2019). This inflammation causes more mucus to be produced in your airways which leads to a wet cough. Again the primary cause of Chronic Bronchitis is smoking since it is not caused by a virus or bacteria, unlike acute bronchitis which can be. In order for the bronchitis to be moved from acute to chronic the individual must have a cough and excess mucus (expectoration) production for most days of at least 3 months a year for 2 years or more in a row. Also, other conditions can cause similar symptoms so those often have to be ruled out before diagnosis. Common tests for Chronic Bronchitis outside of symptoms include Spirometry which is a test that “uses a spirometer device to see how well your lungs are working” (JHM 2019). This may be a recurring test after diagnosis to see how well treatment is working or if the lung disease is progressing. The other common type of test is the peak flow monitor which is a test that “measures the fastest speed you can blow air out of your lungs” (JHM, 2019). The faster you blow the clearer your airways while the slower you blow the more inflamed they may be. Treatment of chronic bronchitis is similar to other conditions under the COPD umbrella but with an added focus on reducing mucus build-up and inflammation.
Asthma
Asthma is a condition in which “your airways narrow and swell and may produce extra mucus” (Mayo Clinic, 2022). Asthma can vary from person to person in strength and symptoms therefore some individuals may go all their life rarely affected by the symptoms while others may have frequent attacks and difficulty breathing. The most common asthma signs are shortness of breath, chest tightness, wheezing when exhaling, coughing or wheezing attaches that are worsened by a respiratory virus. There are also specific types of asthma that flair up in certain conditions such as exercise-induced asthma, occupational asthma, and allergy-induced asthma. You should see a doctor if your signs and symptoms worsen such as when signs and symptoms of asthma become more frequent and intense, you experience increasing difficulty breathing and need to use a quick-relief inhaler more often. Importantly if you experience rapid worsening of shortness of breath or wheezing, no improvement even after using a quick-relief inhaler, or shortness of breath when you’re doing minimal physical activity it may be a sign of an asthma emergency.
Want all this information and more in one easy-to-read guide?
Chronic obstructive pulmonary disease primarily affects the lungs. This is due to the constriction or destruction of the airways and air sacs. As we breathe in air it goes down our windpipe and into tubes called bronchial tubes (often referred to as airways). Inside our lungs, these tubes branch out like a tree into smaller and thinner tubes called bronchioles. Then these tubes end in branches of tiny air sacs called alveoli. You can imagine these as tiny balloons that expand and contract as we breathe. These airways and sacs are typically stretchy as they fill up with air as we breathe in and contract when we breathe out carbon dioxide. However due to COPD less air flows in and out of our lungs. Continuing with the balloon analogy imagine you’re trying to fill up a balloon but there is a hole in it (damaged alveoli) or you’re holding onto the end of it too tight (inflammation in the tubes or alveoli). In the early stages of COPD this results in symptoms such as a nagging cough, shortness of breath, wheezing, and tightness in the chest. These symptoms are where the idea of a “smoker's cough” comes from. Though smokers do make up a lot of COPD cases they are not the only ones. As the disease progresses, the low oxygen in your blood leads to blue/gray lips and/or fingernails, a speedy heartbeat, weight loss, and swelling in the feet and ankles. These extremities are furthest out from the heart and lungs and therefore it takes longer for oxygen to get to them. The heartbeat will increase since due to COPD there will be less oxygen quantity per pump. Meaning your body has to move more blood to keep up with the oxygen needed.
Now that we have covered the basics of how COPD can affect your body, we can now cover its effects on the mind. The lack of oxygen to the brain caused by COPD can have an impact on the brain’s functions and the patient’s mental health. According to the CDC people with COPD may have “overall cognitive impairment or impairment in specific cognitive domains”(CDC,2016). This includes difficulty with processing information, concentration, memory, and self-control. These conditions can cause an individual to become compulsive, unable to stay on task, and forgetful of their surroundings. Since these symptoms are similar to those of dementia, those who develop COPD at an older age may misattribute such symptoms. Furthermore, mental health conditions can develop due to how COPD will affect someone’s day-to-day life. Something as simple as going from the living room to the kitchen for water and back again can become a grueling process with frequent stops to catch their breath. Also if they live in a multistory home, they may have issues getting up and down the stairs which they may have done with ease. This frustration with the disease and its symptoms may develop into feelings of helplessness and depression. These people who were once independent and healthy are now becoming more reliant on others and it can take a mental toll. One way to alleviate this is to make the home more COPD-friendly. Getting different equipment, such as a chair lift, in the home can make it easier for a loved one to get to places they feel they can no longer reach on their own. Another tip is to arrange things so they are easier to access. If you can make it so things they often use are within short distance of each other they are less likely to have an episode or feel needy for asking. Finally, regular outings and socialization are key to promoting a positive mental outlook. These outings should avoid long distances walking since they can flair up their COPD. Take them out to ice cream or a movie, things as small as just going to play cards with them every week can have a major impact on their mental well-being.
Though symptoms can be treated, COPD can not be reversed or cured. Sadly, the lung tissue has already been damaged, and “lung tissue doesn't repair itself.” (Department of Health & Human Service, 2001). The cells that make up your lung tissue are unable to replace the cells that have already been destroyed to create this condition. This often happens due to things such as smoking or inhaling other toxic substances regularly. The effects of COPD can be managed with a variety of treatments and lifestyle changes but can never be fully cured.
MOST IMPORTANTLY QUIT SMOKING
The first step for treatment is to quit smoking. This is a vital step to prevent COPD from getting worse and prevent your lungs from becoming more damaged. There are plenty of nicotine replacement products such as patches and gum to assist with withdrawal symptoms. These are available over the counter at your local pharmacy but for more intense cases of nicotine addiction, it is recommended you talk to your physician for one on one advice. Also, various addiction support groups are out there to aid with the transition/recovery.
Medication
The next step is often one of the different types of medication to assist with the symptoms and complications of COPD. This includes short and long-acting bronchodilators which help relax the muscles around your airways. Bronchodilators are often used to treat long-term conditions, such as COPD, that cause the airways to narrow and inflamed. There are also inhaled steroids that can help reduce airway inflammation and are often prescribed for those with frequent and intense symptoms of COPD. These “corticosteroids, often known as steroids, are an anti-inflammatory medicine” to help reduce inflammation in your lungs (NHS, 2023). Most COPD medications work to reduce the primary symptoms of COPD by reducing inflammation in the airways to promote more efficient breathing. However, there are other treatments for more severe cases.
Lung Therapies
There are also types of lung therapies for those with more moderate or severe COPD. The two most common are oxygen therapy and pulmonary rehabilitation programs. Oxygen therapy helps deliver an increased amount of oxygen to your lungs to assist with loss of breath. This therapy primarily focuses on the issue of not getting enough oxygen in your bloodstream. Depending on the level of COPD a large, in-home unit may be suggested and worn throughout the day and night. However, Small and portable units can assist with shortness of breath when out and about in your daily life. Typically these devices are provided by a Durable Medical Equipment (DME) provider. Furthermore, the size of the oxygen delivery system will vary depending on the low of oxygen needed to stabilize oxygen levels. Pulmonary rehabilitation programs combine exercise training, nutrition advice, education, and counseling. Your doctor will likely refer you to a specialist if this program is recommended. These programs are referred to individuals with worsening COPD and can help prevent hospital readmissions. Another positive impact of these programs is they offer a group setting so you have the chance to meet others with the condition. This can assist with the mental effects of COPD by providing an “opportunity to give and receive peer support” (ALA, 2023). Exercising your lungs, mind, and muscles can help you enjoy activities with your loved ones and make your daily living easier. However, for those with limited success of the above treatments, there is another option.
Lung Surgeries
Finally, there are surgeries available such as lung transplants, bullectomy, and lung volume reduction surgery. Lung transplant surgery is “a surgical procedure to replace a diseased or failing lung with a healthy lung” which often comes from a deceased donor (Mayo Clinic, 2022). This type of surgery is reserved for more severe conditions and when other treatments have not worked or resulted in sufficient improvement. This can be a replacement of just one or both lungs and can involve many complications. The Bullectomy is a surgery where surgeons “remove air pockets in the lungs” (Lung Health, 2023). While these alveoli typically assist in your breathing, by exchanging oxygen from the air with co2 from your blood, damaged ones can form air pockets and need to be removed. Finally, lung volume reduction surgery is when dead or damaged parts of the lung are removed in order to allow the remaining tissue to function better. After lung volume reduction surgery the “diaphragm contracts and reflexes more effectively and efficiently” (Mayo Clinic, 2018). With the damaged part of the lung removed your diaphragm has to move less of your lungs to breathe in and out. All of these surgeries can be used to treat the symptoms of COPD but consult your doctor about the next steps.
What is it?
The COPD action plan breaks down the common symptoms of COPD into three different zones. The green zone is a baseline for a good day, the yellow zone for flare-ups, and finally the red zone for when there is an urgent medical need. Each of these zones also includes helpful steps or actions to take along with making it easy to track what has and hasn’t been done. The second page is a COPD management plan. This management plan includes a variety of medical information about an individual that can be used to recount vital medical information to a doctor or medical professional. Furthermore, some of this data pairs well with the action plan on the previous page. Not to mention there is a QR code at the bottom to access additional resources and video
Why is it helpful?
There are a couple of different things that make this resource useful. The first is the documentation of symptoms and medical information on the management plan. After documenting for a week or so, you or a loved one can better judge the different zones in the action plan. Therefore you can be better prepared for a flare-up or medical emergency. Furthermore, the medical information on the management plan is extremely helpful in communicating your symptoms and baselines to medical professionals. Since everyone’s experience with COPD is different what may seem like a minor change for some could be big for others. It also makes things easier if the individual with COPD is experiencing a mental haze to have all this documented. Also if multiple different medical professionals (DME, Home Care, PT/OT, etc.) are assisting in care for yourself or a loved one then this assists with clear communication between them. The second benefit of this document is the clear green, yellow, and red system. It can be difficult to differentiate how COPD is affecting someone day to day and to communicate that well. The American Lung Association has made it easier along with action steps to fit the different zones based on how they are feeling. Also, you can personalize each of these steps and actions in accordance with what fits you or your loved ones best. Such as how often to take their inhaler, what medications they may be on, etc.
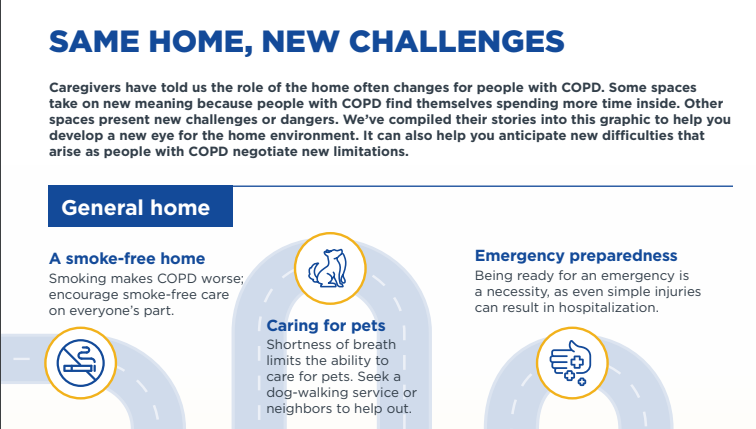
What is it?
This resource/module is broken down into eight parts to assist with making a home/living space accessible and safe for a loved one with COPD. The first section covers the challenges you or a loved one may experience in the home. This includes some general tips and reminders about how to make the home a bit safer for a loved one with COPD. The next section covers the first steps you should take to move towards a safer home including removing indoor triggers and managing the effects of smoke and radon. The third section then covers how to best manage oxygen supplies if your loved one is on oxygen. Section four covers medication organization and management. Section five moves towards the outdoors which is also continued in section six. Finally sections seven and eight cover specific tips for warm and cold weather since they impact COPD and its symptoms differently.
Why is it helpful?
This is a useful document since a loved one’s environment can have a large impact on their condition and treatment. Small changes can seem unimportant but they could prove to be important when it comes to a loved one’s health and safety. Removing and managing certain triggers can make it so your loved one has flair-ups less often. Also, the advice on storing/managing medications can be extremely useful because the forgetfulness that can develop from COPD may result in mixed or missed medications. Not to mention the in-depth assistance on oxygen equipment storage and maintenance. Oxygen therapy can not only be ineffective if not done properly but can potentially lead to further damage or infections if not handled correctly. Also, the tips can help prevent the ignition of the gas or tanks since oxygen is flammable.
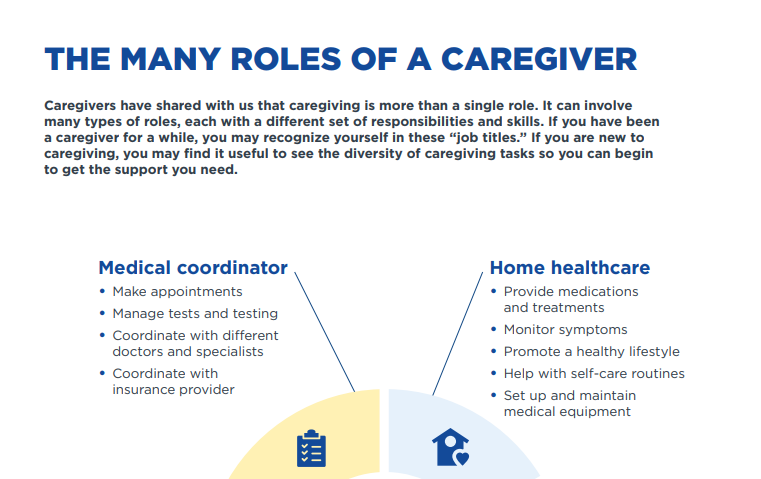
What is it?
This resource covers the different roles a caregiver of COPD fulfills while caring for a loved one. From guardian to support system to family member, there are many roles you will often try to fill at once. The most important part this resource covers is taking care of your mind and body while doing so. This section includes warning signs of anxiety, depression, and stress. Next, the resource covers some of the different support networks out there and how to find the right one for yourself. Finally, it covers how to build up a care management team to take some of the burden and roles off of yourself. This also includes navigating changing relationships and roles for yourself.
Why is it helpful?
Often caregivers of a loved one neglect their own well being order to care for another. Sometimes they don’t realize this until it is too late and suffer from caregiver burnout. It is vital for your own and loved one's health that you take care of yourself. You can’t take care of someone properly if you are overwhelmed or stressed out by a situation and the large amount of energy it may require. If you notice yourself being short with a loved one or rushing certain tasks out of frustration, it may be time to take a step back and read over this resource. After following the steps in this resource, you can work to not only take care of your loved one but also build up a support network for yourself.
What is it?
Simply put this is a quick overview of what palliative care is and how it can assist someone with COPD. The document gives advice on why you may want palliative care, how to get it, and how to pay for it. It also has some handy questions that are often asked about Palliative care with their answers.
Why is it helpful?
Palliative care is a term thrown around a lot but is never clearly defined/explained. This resource does so and provides answers to many of the common questions you or a loved one may have when it comes to palliative care. Palliative care can be a great resource to alleviate stress for both the one with COPD and their caretaker(s).
What is it?
If you’re looking for a deep dive into the scientific and medical side of COPD then you will want to look here. The CDC has compiled its reports, articles, and resources all into one page, This includes reports on COPD, COPD treatments, and COPD advocation. The first two resources are ways for you to get involved in the CDC’s advocacy of COPD. The page is also broken down into general information, rehabilitation, self-management, and patient support groups.
Why is it helpful?
The CDC is always an excellent and trusted resource for information on diseases, their effects, and their treatments. This information can be extremely useful when caring for a loved one with COPD or talking to a loved one about it. The only downside is it is very text-heavy and full of scientific terms so it’s best to take it in bite-sized pieces over time so you can more easily process what you’ve learned.
Conclusion
In conclusion, Chronic Obstructive Pulmonary Disease is a term used to cover a variety of medical conditions affecting your lungs. These diseases not only affect your body through difficulty breathing but also the functions of the body that are sensitive to oxygen loss. Not to mention the added effects of the disease on the mind and how it can lead to memory loss and mental health conditions if not treated right. Speaking of treatment there are a variety of them out there so it's best to start with the cause and work up from there.
Hopefully, we have now thoroughly informed you about COPD. Below is a copy of our most recent guide on COPD which includes:
- The information above (in a convenient document)
- Additional Resources (Community Resources, Helpful Blogs, etc)
- And an extra section on what to do when COPD worsens (Not available elsewhere)
Sources:
Centers for Disease Control and Prevention. (2023, June 30). Chronic obstructive pulmonary disease (COPD). Centers for Disease Control and Prevention. https://www.cdc.gov/copd/index.html#:~:text=What%20is%20COPD%3F,includes%20emphysema%20and%20chronic%20bronchitis.
Centers for Disease Control and Prevention. (2016, January 7). Association of chronic obstructive pulmonary disease with increased confusion or memory loss and functional limitations among adults. Centers for Disease Control and Prevention.
Association, A. L. (n.d.). Emphysema. American Lung Association. https://www.lung.org/lung-health-diseases/lung-disease-lookup/emphysema#:~:text=Emphysema%20is%20one%20of%20the,alveoli%20(tiny%20air%20sacs).
Chronic bronchitis. JHM. (2019, November 19). https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-bronchitis#:~:text=Chronic%20bronchitis%20is%20often%20part,may%20also%20play%20a%20role.
Mayo Foundation for Medical Education and Research. (2022, March 5). Asthma. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/asthma/symptoms-causes/syc-20369653
Department of Health & Human Services. (2001, November 28). Lung conditions - chronic obstructive pulmonary disease (COPD). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/lung-conditions-chronic-obstructive-pulmonary-disease-copd
Mayo Foundation for Medical Education and Research. (2022, December 14). Lung Transplant. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/lung-transplant/about/pac-20384754
Health, S. V. H. (n.d.). Home. St Vincent’s Lung Health. https://www.svhlunghealth.com.au/procedures/procedures-treatments/bullectomy
Mayo Foundation for Medical Education and Research. (2018, November 16). Lung Volume Reduction Surgery. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/lung-volume-reduction-surgery/about/pac-20385045
Corticosteroids. NHS inform. (2023, June 15). https://www.nhsinform.scot/tests-and-treatments/medicines-and-medical-aids/types-of-medicine/corticosteroids#:~:text=Corticosteroids%2C%20often%20known%20as%20steroids,on%20top%20of%20the%20kidneys).
Association, A. L. (2023, March 10). The Basics of Pulmonary Rehabilitation. The Basics of Pulmonary Rehabilitation | American Lung Association. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/pulmonary-rehab