You Don't Need to Be a Nurse To Understand Parkinson’s
First off, what is Parkinson’s Disease?
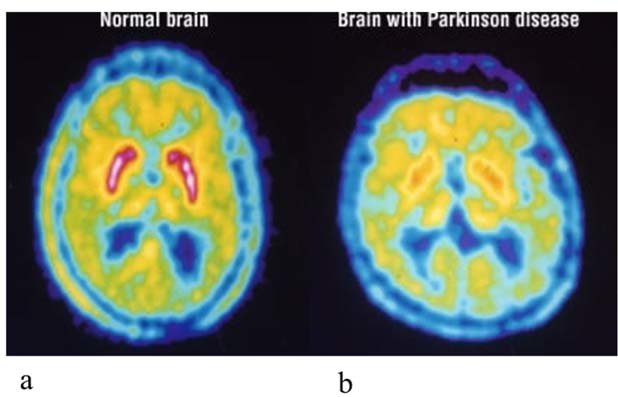
Parkinson's disease is a chronic, progressive brain and nerve disease that affects a small area of nerve cells (neurons) in an area of the brain known as the substantia nigra. These cells normally produce dopamine, a chemical (neurotransmitter) that transmits signals between areas in the brain. These signals, when working normally, coordinate smooth and balanced muscle movement. Parkinson's disease, however, causes the neurons in the substantia nigra to die, leading to a lack of dopamine in the brain. The loss of dopamine leads to a loss of the ability to control body movements normally. This is often displayed in tremors or “freezing” while trying to walk or get up.

What Causes Parkinson's?
The exact cause of Parkinson’s disease is unknown but several key factors play a role. Researchers have identified specific genetic mutations that can cause Parkinson’s disease. However, they are uncommon except in rare cases with many family members affected by Parkinson’s disease. This research has also shown that certain gene variations appear to increase the risk of Parkinson’s disease but with a relatively small risk of Parkinson’s. Researchers have also noted that many changes occur in the brains of people with Parkinson's disease, although it's not clear why these changes occur. These changes include The presence of Lewy bodies. Clumps of specific substances within brain cells are microscopic markers of Parkinson's disease. These are called Lewy bodies, and researchers believe these Lewy bodies hold an important clue to the cause of Parkinson's disease. Alpha-synuclein is found within Lewy bodies. Although many substances are found within Lewy bodies, scientists believe an important one is a natural and widespread protein called alpha-synuclein (a-synuclein). It's found in all Lewy bodies in a clumped form that cells can't break down. This is currently an important focus among Parkinson's disease researchers.

What Are Some Of The Common Risk Factors?
Age. Young adults rarely experience Parkinson's disease. It ordinarily begins in middle or late life, and the risk increases with age. People usually develop the disease around age 60 or older. Heredity. Having a close relative with Parkinson's disease increases the chances that you'll develop the disease. However, your risks are still small unless you have many relatives in your family with Parkinson's disease. Gender. Men are more likely to develop Parkinson's disease than are women. Exposure to toxins. Ongoing exposure to herbicides and pesticides may slightly increase your risk of Parkinson's disease.

What are the Early Warning Signs/Symptoms?
There are a wide variety of early warning signs. The first and most obvious is tremors. you or a loved one may have noticed a slight shaking or tremor in your finger, thumb, hand, or chin. A tremor while at rest is a common early sign of Parkinson's disease. Shaking can be normal after lots of exercise, if you are stressed or if you have been injured. Shaking could also be caused by a medicine you take. A second warning sign is small handwriting. Those suffering from Parkinson’s may notice the way they write words on a page has changed, such as letter sizes are smaller and the words are crowded together. A change in handwriting may be a sign of Parkinson's disease called micrographia. However, sometimes writing can change as you get older, if you have stiff hands or fingers or poor vision. A third warning sign is loss of smell. Have you noticed you no longer smell certain foods very well? If you seem to have more trouble smelling foods like bananas, dill pickles, or licorice, you should ask your doctor about Parkinson's. Your sense of smell can be changed by a variety of factors including cold, flu, or a stuffy nose, but it should come back when you are better. A fourth warning sign is difficulty sleeping. Do you thrash around in bed or act out dreams when you are deeply asleep? Sudden movements during sleep may be a sign of Parkinson's disease. It is normal for everyone to have a night when they 'toss and turn' instead of sleeping. Similarly, quick jerks of the body when initiation sleep or when in lighter sleep are common and often normal. A fifth early warning sign is trouble moving or walking. Do you feel stiff in your body, arms, or legs? Have others noticed that your arms don’t swing as they used to when you walk? Sometimes stiffness goes away as you move. If it does not, it can be a sign of Parkinson's disease. An early sign might be stiffness or pain in your shoulder or hips. People sometimes say their feet seem “stuck to the floor.” However, If you have injured your arm or shoulder, you may not be able to use it as well until it is healed, or another illness like arthritis might cause the same symptoms. A sixth early warning sign would be constipation. Do you have trouble moving your bowels without straining every day? Straining to move your bowels can be an early sign of Parkinson's disease and you should talk to your doctor. Also If you do not have enough water or fiber in your diet, it can cause problems in the bathroom. Also, some medicines, especially those used for pain, will cause constipation. If there is no other reason such as diet or medicine that would cause you to have trouble moving your bowels, you should speak with your doctor. A seventh early warning sign is a soft or low voice. Have other people told you that your voice is very soft or that you sound hoarse? If there has been a change in your voice you should see your doctor about whether it could be Parkinson's disease. Sometimes you might think other people are losing their hearing when really you are speaking more softly. However a chest cold or other virus can cause your voice to sound different, but you should go back to sounding the same when you get over your cough or cold. An eighth warning sign is a masked face. Have you been told that you have a serious, depressed or mad look on your face, even when you are not in a bad mood? This is often called facial masking. If so, you should ask your doctor about Parkinson's disease. Some medicines can cause you to have the same type of serious or staring look, but you would go back to the way you were after you stopped the medication. A ninth warning sign is a dizziness or fainting. Do you notice that you often feel dizzy when you stand up out of a chair? Feeling dizzy or fainting can be a sign of low blood pressure and can be linked to Parkinson's disease (PD). Everyone has had a time when they stood up and felt dizzy, but if it happens on a regular basis you should see your doctor. A tenth warning sign is stooping or hunching over. Are you not standing up as straight as you used to? If you or your family or friends notice that you seem to be stooping, leaning, or slouching when you stand, it could be a sign of Parkinson's disease (PD). If you have pain from an injury or if you are sick, it might cause you to stand crookedly. Also, a problem with your bones can make you hunch over.
Are There Other Conditions Linked to Parkinson’s?
Parkinson’s Disease can also lead to conditions Including Neurogenic Orthostatic Hypotension (nOH). Orthostatic hypotension (OH) is a persistent drop in blood pressure that occurs upon moving from sitting to standing or from lying down to sitting up or standing. Doctors define it as a blood pressure drop of 20 millimeters of mercury (20 mm Hg) in systolic blood pressure (the top number in a blood pressure reading), or a drop of 10 millimeters in diastolic blood pressure. When OH happens in people with PD or other nervous system disorders, it is called neurogenic OH (nOH). Damage caused by these disorders, including PD, can result in the nervous system not being able to make or release norepinephrine — a chemical that constricts blood vessels and raises blood pressure. This causes dizziness or lightheadedness. The range of people affected by nOH is large; estimates suggest anywhere from 10 to 65 percent of people with PD develop nOH. This symptom is common in mid-and late-stage Parkinson’s, but can also happen earlier in the disease. OH, symptoms include Lightheadedness, Dizziness, Weakness, Difficulty thinking, Headache, and Feeling faint. Another condition that can affect people with Parkinson’s is Pseudobulbar Affect (PBA). Pseudobulbar affect (PBA) is characterized by frequent, uncontrollable outbursts of crying or laughing. It happens when a nervous system disorder, such as PD, affects the brain areas controlling the expression of emotion. This disrupts brain signaling and triggers involuntary episodes. Outbursts are usually brief, though they can be intense and may occur several times per day. PBA is often mistaken for depression or bipolar disorder. The episodes often do not match the situation or the person’s feelings. You may be happy about something but start sobbing, or laugh in an inappropriate situation. PBA used to be referred to as “emotional incontinence” or “pathological laughing and crying.” These terms are not commonly used today because researchers better understand the brain and PBA symptoms. Pseudobulbar affect can also occur in people with brain injuries. According to PBA Info, up to 24 percent of people with PD have symptoms that may suggest PBA.
Ok, But How Can I Manage Parkinson’s?
Exercise helps manage Parkinson’s symptoms. Exercise is vital to maintaining balance, mobility, and activities of daily living. There are a number of different types of exercise, and each kind can benefit a person with PD. In addition to a variety of types of exercise, consistency and intensity are also important to get benefits from exercise. People with PD who have participated in regular exercise for durations longer than six months have seen significant progress and benefits. The intensity of the exercise is measured by how much it increases heart rate and respiration rate. People with PD who exercise with intensity experience greater benefits. Recent research indicates that high-intensity interval training may be more effective than longer periods of moderate intensity. Even people in advanced stages of the disease can participate in these high-intensity programs. Balance exercises are those that aim to improve balance and increase lower body strength. Balance exercises are particularly important to reduce the risk of falls by improving the way a body can adjust and maintain its position. Strengthening exercises build muscle mass, which improves the ability to perform many daily activities, like standing from a chair. Strength exercises usually focus on one part of the body, such as arms or legs, and should be rotated to exercise all the major muscle groups. Strengthening exercises use weights or resistance, and they may also be called resistance exercises. Endurance exercise, or cardiovascular exercise, raises the heart rate and breathing for an extended period of time. Examples of endurance exercises are walking, jogging, swimming, and dancing. This kind of exercise is also called aerobic activity. Flexibility exercises are those that focus on stretching and maintaining movement and range of motion. Maintaining flexibility is critical to maintaining the ability to perform daily activities like reaching for objects from a shelf and getting dressed.5
Some types of exercise have shown particular benefits to the needs of people with Parkinson’s including Cycling, such as on stationary bicycles, which helps reduce the symptoms of PD, particularly when cycling at higher rates. Dancing helps people with PD maintain mobility, flexibility, and balance. Some people with PD find that playing sports helps them stay active and maintain their mobility. Sports that people with PD have found beneficial include boxing, swimming, and gymnastics. A great program for those with Parkinson’s is the Rock Steady Boxing program which has over 700 gyms across the globe. “Rock Steady Boxing is a nonprofit gym that provides an effective and fun exercise program for people living with Parkinson’s disease. Studies suggest that intense exercise programs may be ‘neuroprotective’ actually working to delay the progression of symptoms.” The cost of membership is $100 per month.
Is There A Way To Prevent It?
Because the cause of Parkinson's is unknown, proven ways to prevent the disease also remain a mystery. Some research has shown that regular aerobic exercise might reduce the risk of Parkinson's disease. Some other research has shown that people who consume caffeine — which is found in coffee, tea, and cola — get Parkinson's disease less often than those who don't drink it. Green tea is also related to a reduced risk of developing Parkinson's disease. However, it is still not known whether caffeine actually protects against getting Parkinson's, or is related in some other way. Currently, there is not enough evidence to suggest drinking caffeinated beverages to protect against Parkinson's.
Are There Treatments?
There is no one-size-fits-all treatment approach when it comes to Parkinson’s. Some common treatments include Dopamine promoter medications to counteract the loss of dopamine emitters due to the disease. Other symptoms countering medications include antidepressants, cognition-enhancing medications, and anti-tremor medication. All of which may or may not be prescribed based on your loved one’s symptoms. One of the current treatments is Deep brain stimulation (DBS) is a treatment for symptoms of Parkinson's disease, including tremors, stiffness, and trouble walking. It can also treat the side effects of Parkinson's medicines. DBS isn't a cure for Parkinson's and won't stop it from getting worse. But it may be an option if you've had the disease for at least 5 years and don't get enough relief from medicine. For some people, DBS is life-changing. For others, the results aren't as good. If it doesn't help you, your doctor can take the device out. How does it work? A small device placed inside your chest sends electrical pulses to your brain. The pulses block nerve signals that cause Parkinson's symptoms. A DBS system has four parts a thin wire, called a lead, that's placed in the part of your brain causing symptoms, a pulse generator, like a pacemaker, that sends tiny electrical signals to the lead, a wire that connects the lead to the pulse generator and remote control to program the system -- the only part outside your body. After the system is in place and turned on, a DBS expert will adjust it so you get the best relief for your symptoms. You can also control the system yourself. You can turn it off and on, check the battery, and tweak the settings. Therapy can help a lot with the mental symptoms of Parkinson’s disease. Talking to a licensed therapist about the mental challenges you are facing and the emotions you are feeling can help put your mind more at ease. These individuals are also extremely skilled in helping you develop skills to manage depressive or emotional flare-ups on your own. Another treatment is Guided Imagery. Guided imagery is a proven form of focused relaxation that helps create harmony between the mind and body. Guided imagery coaches you in creating calm, peaceful images in your mind -- a "mental escape." This technique, which can aid any treatment or procedure, provides a powerful psychological strategy that enhances a person's coping skills. Many people dealing with stress feel loss of control, fear, panic, anxiety, helplessness, and uncertainty. Research has shown that guided imagery can dramatically counteract these effects. It can help people overcome stress, anger, pain, depression, insomnia, and other problems often associated with illnesses and medical/surgical procedures. It is clear that stress and depression can worsen the symptoms of Parkinson's disease. By using guided imagery, you can stay calm.
What Should I Do Now?
Taking action early will enable you to understand and deal with the many effects of your condition. A mental health care provider can design a treatment plan to meet your specific needs. Strategies can be designed to help you regain a sense of control over your life and improve your quality of life. Other steps include finding out as much as you can about the illness. You can go to parkinson.org or ask your family doctor about the disease. Do not be afraid to ask your doctor, nurse, or other health care provider to repeat any instructions or medical terms that you don't understand or remember. They should always be available to answer your questions and address your concerns. One step is to make use of resources and support services offered by your hospital and in your community. These can also include the resources provided by the Parkinson’s Foundation. Another step is to talk to your friends and family about it. Don't isolate them. They will want to be involved in helping you. It is also a very important step to continue to do things you enjoy. To keep your quality of life, do not give up on your passions and hobbies. A final step is to keep up your mental health. Learn to manage stress. This will help you to maintain a positive physical, emotional, and spiritual outlook on life. Being stressed out will only make the situation worse. You should try to organize a daily routine that will reduce stress, with downtime for both you and your family members. If you are depressed -- and this is more than just feeling sad occasionally -- antidepressants can be prescribed to help lift your mood or therapy can help you better cope with your symptoms.
How Can I Help A Loved One With Parkinson’s?
One important way to help a loved one with Parkinson’s is to learn about the disease, so you can be better informed of their journey. As time goes on you will be able to more easily adapt and aid your loved one more since you will know what to expect. We suggest you take a look at websites such as the Parkinson’s Foundation and attend medical appointments with your loved one. Don’t be afraid to ask medical professionals questions about the disease and its management, they should be happy to help. The next important step is to listen to your loved one. Sometimes the best way to help someone is to give them someone. It may take some time for your loved one to open up about their feelings but either way, it is often a weight taken off them. Another step you can take to help is to help them feel normal. Do not constantly mention the disease in discussions with them or how bad they must feel, instead try and focus on things that make them happy or share stories with each other. Also, do your best to keep them involved in family activities as they did before. A final step is to be active with them. Encourage your loved one to keep active with you, this could be taking a yoga class together or even just a simple walk around the neighborhood. Fitness improves strength, balance, memory, and quality of life in people with this condition

Matthew Laming
Client Relations Specialist at GLHCU
Graduate of Northwood University