When many people begin their search for a home health care agency they are often inexperienced and can easily get lost with all of the different duties that have been thrust upon them. Between trying to care for their loved ones and maintaining their home life it is hard to do the research needed to find the right kind of care for a loved one. That is where this small, handy list of questions can come in and help. We have compiled a list of 10 questions that we are often asked when interviewed as a home care company plus a bonus question we feel is essential to ask every company you work with! We at GLHCU have also added a reason why you should ask each question and our responses to them.
1) What is your agency's plan for if a caregiver calls off?
Why ask this question: It is important to know if the agency has a backup plan. Caregiver call-offs are inevitable, even the best caregivers have to call in from time to time. Most companies will have a caregiver or two who are a good fit for the home as back up and hopefully, they have trained with your loved one or been to the home before. It is also a good time to ask how many caregivers they have in the area or which caregivers they have in mind for your home. This question is also essential because if the company does not have a back up they may require you or another loved one to stay with the client instead.
Our Response: It is always our goal to have a backup plan if a caregiver is unable to make a shift. We have multiple caregivers across the state who can fill a variety of shifts. We also don't take a case unless we have the needed caregivers and backup caregivers ready to work (Typically 2 for cases with fewer hours, all the way up to 6 caregivers for a 24/7 case). We then continue to hire in the area to build up a pool of local caregivers who can pick up a shift whenever needed. As a last resort, we have proven caregivers who are willing to travel further to help out our clients in need. Though these caregivers would prefer to work closer to their homes, they are often ready and willing to help out at a moment's notice.
2) How do you provide credible caregivers?
Why ask this question: In-home care is a very personal service and sometimes your loved one is in a very vulnerable state due to their condition(s). You are not just having someone come and provide a service but also trusting them to take care of your loved one. With all of these factors, a company must provide credible caregivers. Ask them about their vetting process and how they make sure your loved one is safe with these people in their home. Yes, they may say that they do a background check and drug screen, but how in-depth is it? Some checks are limited to a county while others are for the whole country. Also, some drug tests only test for a few items while others test for a large variety. You do not want someone in your loved one’s home who has a behavior pattern of stealing or is continually under the influence of some drug.
Our Response: Though not all of our caregivers are licensed, such as CNA or MA, most of our caregivers have years of experience in the field. Before we hire anyone we conduct a full reference check. This includes calling their previous employment and personal references. We also only hire caregivers that pass a national background check, sex offender registry check, the office of inspector general check, and finally, a 13-panel drug test. All of these checks are done yearly and we do reserve the right to randomly drug test if needed. We also verify all caregivers have a valid driver's license and auto insurance.
3) How do I know if my caregiver is working the hours they are supposed to, and how can I get status updates on the services they are providing to my loved ones?
Why ask the question: This is especially important when a loved one does not live with you or care is provided when you are not in the home. It can often be hard to know if your loved one is getting the proper care or even if the caregiver was there. Now, most companies will have some form of the way for caregivers to clock in and out but the systems vary in reliability and detail. Most programs do require a call in from a preselected line or some even are GPS enabled and limit clock in/out to a specific range of the address. Also, a proper company will have signed documentation of what they are doing for your loved one. These records should be available to family members or some even leave a carbon copy in the home upon request.
Our Response: We schedule our caregivers a month in advance and provide a schedule to the household/family every month. Our system also has a family portal. This is where you can monitor the care of your loved one. This portal has a live schedule, a feed of what tasks have and have not been completed in the home, and the option to add notes or special tasks. All communication in the portal goes directly to our staff who can answer any questions you may have about your loved one and their care. Our caregivers are required to clock in and out either via a smartphone with GPS tracking or our telephony system. This is all to make sure that your loved one gets the care they need. Finally, all of our caregivers are required to fill out a home visit record/note that details their shift.
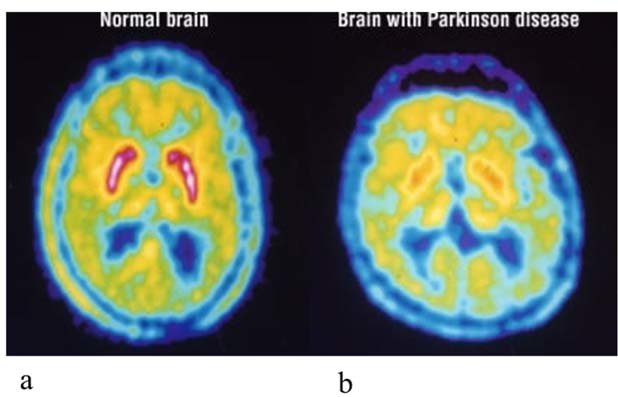
4) Can I get a caregiver who has experience with a specific disease or disability?
Why ask the question: The same reason you would not ask someone who can’t cook to cater your wedding. Yes, they can do it, but you may all be eating grilled cheese and tomato soup. All jokes aside, it is important to ask this question if you have someone with a specific disease or disability (Including but not limited to Dementia, Parkinson’s, and Traumatic Brain Injury). Yes someone without experience with a specific disease can still care for someone who needs the specialized help, but they often lack the tools those who have experience can call upon.
Our Response: Absolutely! We make sure to match up a caregiver's experience with the home. For example, a client with dementia will receive a caregiver with dementia experience. If a caregiver needs a refresher or has limited experience with a disease we make sure they are fully trained by our Nursing Supervisor before they are sent to the home.
5) How quickly will a provider be able to respond in an emergency?
Why ask the question: Emergencies happen. Whether it is a medical emergency for the patient or a natural disaster, a care company should always have some form of a plan. If they do, you may even want to request a copy of their procedures. Most companies will have a plan they can produce for you within a few hours. Most companies will have some form of on-call but if you have an important medical question you may be SOL if they don’t have a nurse available.
Our Response: In the case of a medical emergency, the client, caregiver, or family should call 911 before contacting us. However, we have a 24/7 on-call staff that can answer any questions you have or any other issues that may arise. This includes situations such as if a caregiver does not show up or you have an important schedule change. On top of that, we have a licensed nurse who can answer any medical questions at a moment’s notice. We work hard to make sure that you are kept up to date and your loved one is cared for, even after "normal" business hours. On top of that, we have a what to do in case of an emergency sheet in every one of our binders in a client’s home, so our caregivers can reference it if they are ever lost on how to act.
6) Can your agency provide any references?
Why should you ask this question: Established companies should be able to provide a list of references. If they aren’t able to, it may be a concern. Yes, HIPPA laws will prevent them from just giving you a list of current clients, but those that have been providing quality care for a while should at least have a few people who have volunteered to be referenced for potential clients. These references should easily be able to answer any of your questions about the company and receiving services from them. A bonus would be clients who have similar conditions to your loved ones.
Our Response: Absolutely, we have a few different clients who have offered to be a reference for us and our caregivers. They have offered to talk to others about the services we provide and their experience as a client of our company.
7) How do the agency train and monitor caregivers? Does the agency provide continuing education?
Why ask the question: Training can be crucial for new caregivers entering the field and therefore crucial to the care of your loved one. Newer caregivers will need training on basics and most companies should have some form of a training program, especially one put on by a nurse. This is where caregivers can pick up on skills such as taking manual blood pressures, using a gait belt, and more. On top of that, a company should have a continuing education program to help their caregivers and nurses stay up to date on their training and advancements in the field.
Our Response: We currently have a training program in place for all of our employees run by our head registered nurse. There she walks our caregivers through all of the essential tasks they should know how to do before going out into the field. If there is a more specific skill a caregiver has to learn before entering a home for work, she will teach them one on one until they have a solid grasp on how to do it. Some training may even take place in the home to get a caregiver familiar with the tools in the home and the client. Continuing education is provided for our licensed caregivers and nurses. They complete modules online to further their education and stay on top of advances.
8) What resources does the agency provide for financial assistance, if needed? For instance, is a payment plan available?
Why ask the question: Getting care for a loved one can be a little expensive depending on the level of care, the company, and a few other factors. That is why it is important to ask if companies have a way to financially assist you. This can include what type of insurance they take if any fees apply if a client is not able to pay their bill on time due to financial issues and if payment plans are available. You may also want to ask how flexible the company is on hours and days, if the financial burden is too much could you decrease hours without penalty?
Our Response: We work with a wide variety of insurances, claims adjusters, and payer sources to make in-home care more affordable for our clients. Our billing department is always happy and willing to help in any way possible. If the client is a veteran, we work with the Department of Veteran’s Affairs and provide informative literature about the different benefits a veteran or surviving spouse can receive. If your loved one needs care due to an auto accident or has a long-term care insurance policy, we work hard with insurance and claim adjusters to make sure your loved one’s care is paid for. We take all the hassle of such by working directly with those companies and providing supporting documentation so your loved one gets continued care.
9) Will you receive a written care plan before service begins?
Why ask the question: The care plan should include details about medical equipment, specific care needs, and responsibilities of the aide or agency. It should also contain input from the doctor, and be updated frequently. Care plans are meant to be a resource for all aids coming into the home and often also contain what tasks are asked of the caregiver. These should also include emergency contact information and be easily accessed by a caregiver.
Our Response: Though we do not typically send a plan of care to relatives before starting care, one is always in the binder we keep in each home. We will gladly send one upon request. After an initial assessment, the information will be put into our scheduling system and a plan of care will be created and sent to the home before care starts. Our caregivers have access to this before they go to their shifts and are advised to read over it before starting their shifts. These care plans are updated yearly or if a major change happens in a client’s life or needed care. These plans of care also have emergency contact information at the top so a caregiver can contact you in case of a medical emergency.
10) How are problems addressed and resolved? Whom can you or another family member contact with requests, questions, or complaints? Will the agency work directly with you or your loved one, family members, and health care providers?
Why ask the question: This is essential because communication is key. Problems can arise with such a personal service. Some family members, yourself, or the client may not be happy with the way services are currently being provided. You may also not like a certain caregiver or there may be a conflict between the client and caregiver. If such problems arise it is important to know who you need to talk with to resolve these issues. It is also key to know how such problems are resolved. Do they just get put in a book and dismissed or are they fully investigated and properly resolved. Some companies may even just say you have to deal with it. As far as working with others, a good home care company should be communicating with all individuals involved. This communication has to be clear and speedy to solve any problems and make sure your loved one gets the best care.
Our Response: As far as any employee and client conflicts we have a few different approaches. The most common one is if a client does not want a caregiver back or the caregiver wishes to not return then we mark so in our system and take said caregiver off the schedule. In more serious cases the authorities may need to be involved and a dissolvent of the relationship may need to take place (whether caregiver to company or client to the company). We never want to put your loved one or our caregivers in harm's way. All such requests or complaints will be directed toward or office staff who will handle the situation. If you have questions about a specific topic, we provide a list of our employees and their specialty at the time of a client opening. Therefore you are educated on who to contact with your questions or we at the office can direct your call as well. All medical questions will be answered by our on-call registered nurse who will update you and the plan of care as needed. Finally, our scheduling system allows you to have access to what is going on in the home while our caregivers are there. Our caregivers can leave notes on how the shift went and if there was any cause for concern with the client. These notes are available in the client portal and if there is a change in the client's condition, our nurse and office staff are immediately notified through our system or the caregiver often calls to let us know. This information is all relayed to those involved in the client’s care.
Bonus Questions: Why was your company founded?
Why ask the question: This can give you an idea of the people behind the company and its story. Some people are just in it for the money, plain and simple while others have a solid reason behind why they decided to start a company and provide care to others. These stories are often more than just they like to help others or like working with the elderly. Those who are in it for the money often make less empathetic decisions and care more about the profit than the client and caregivers. However, those who have a solid reason to be in business are typically the ones who go above and beyond because they were in your shoes once or currently still are.
Our Response: For over 30 years Matt & Beth have been the caregivers for their handicapped son. They've had to deal with companies that provided caregivers & nurses that were unreliable and unskilled. That's why they created Great Lakes Home Care Unlimited 7 years ago. They knew others deserved better care and to be treated like family. We understand what it is like to be in your shoes and have to care for a loved one. It is the reason we get up and work hard to give people the kind of care they deserve, every day!








Recent Comments